Characteristics of the couples seeking IVF treatment
There are many factors that may affect the outcome of IVF treatment. These may include one of the following characteristics of the couples seeking IVF treatment.
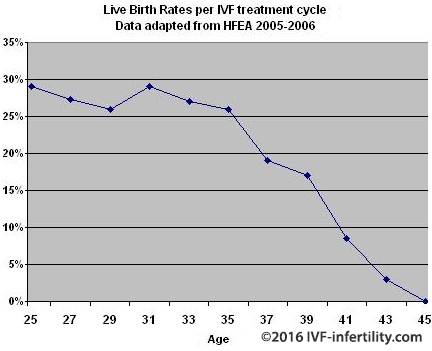
The age of the woman
The age of the woman has a significant affect on her fertility and the live birth rate decreases significantly from the age 35 years when the woman is using her own eggs. The older the woman, the higher the chance of cancellation, the lower the chance of success and the higher chance of miscarriage and chromosomal abnormalities. In the USA the live birth rate of women aged 41 and over was 7.1% per cycle initiated.
| Age group | Less than 35 | 35-37 | 38-40 | 41-42 |
| Pregnancy | 43.1% | 35.7% | 26.8% | 17.6% |
| Live birth | 37.3% | 29.5% | 19.7% | 10.6% |
Data adapted from SART report 2005.
Approximately 12% of all IVF cycles are cancelled before egg collection. The main reasons for cancellation are no or poor egg production (83%), patient’s personal reasons (10%), excessive response to ovarian stimulation and risk of developing OHSS (5%), medical illness (1%). Adapted from SART 2005 and HFEA 2006 Reports.
| Womens age | Cancellation rate |
| Less than 35 | 7.7-10% |
| 35-37 | 11.6-14.7% |
| 38-40 | 14.6-19.5% |
| Over 40 | 19.1-24.6% |
Data adapted from SART report 2002
Use of donated eggs, donor embryos or donor sperm
The highest live birth rates are found among women who have had IVF with donated eggs, donor sperm or donated embryos.
Live birth rate per cycle in couples who have had IVF with their eggs and sperms compared with IVF using donor sperm, donated eggs and donated embryos. The overall delivery rate per transfer following the use of donor eggs was 41.2% compared to 31.1% following IVF using own eggs (data from SART report 2002).
| Own eggs and sperm | 15.4% |
| Own eggs and donor sperm | 19.9% |
| Own sperm and donated eggs | 21.9% |
| Donated eggs and donor sperm | 22.2% |
Data adapted from HFEA Report 1997
Number of embryos transferred
In the United Kingdom, a maximum of three embryos may be replaced per treatment cycle for women aged 40 or older at the time of embryo transfer but for women aged 39 years and younger, the maximum is two embryos (HFEA, code of practice, 7th edition. London. 2007). The aim is to reduce the risk of multiple pregnancy
| Number of embryos replaced | Live birth rate per cycle | Multiple pregnancy rate |
| One | 6.8% | 4.7% |
| Two | 16.8% | 24.3% |
| Three | 21.4% | 32.6% |
Data adapted from HFEA Report 1997
There is some evidence that the live birth rates for treatment where two embryos are transferred (provided that more than four embryos were created) is almost identical to the live birth rate for treatments where three embryos are transferred but with a lower multiple pregnancy rate.
| Number of embryos replaced | Live birth rate per cycle | Multiple pregnancy rate |
| Two | 26.4% | 26.0% |
| Three | 26.0% | 34.3% |
Data adapted from HFEA Report 1998
Currently, an increasing number of IVF centers world wide advocate elective single embryo transfer (eSET) for selected patients, who are most likely to conceive after IVF treatment (woman aged 35 or younger, first IVF treatment and who have several good quality embryos available for transfer). The aim, again, is to reduce multiple pregnancy rates.
Overall, eSET has success rates comparable to double embryo transfers if cumulative pregnancy rates are calculated from both fresh and subsequent frozen transfers. In the United KIngdom, the twin pregnanct rate was reduced to only 11% and in the USA was 13 % with less than 1% triples or higher (SART and HFEA 2018).
Duration of infertility
The longer the couple has been infertile, the lower the chance of success.
| Duration of infertility | Live birth rate per embryo transfer cycle |
| 1-3 years | 19.5% |
| 4-6 years | 18.7% |
| 7-9 years | 17.0% |
| 10-12 years | 16.4% |
| Over 12 years | 11.8% |
Data adapted from HFEA Report 1999
Cause of infertility
Outcome of IVF treatment varies with the cause of infertility.
| Cause of infertility | Live birth rate per embryo transfer cycle |
| Tubal | 13.3% |
| Endometriosis | 15.0% |
| Unexplained | 15.9% |
| Male | 19.6% |
The presence of severe endometriosis is associated with poor clinical pregnancy rates in women undergoing IVF (Harp et al BJOG 2014).
Data adapted from HFEA Report 1997
Number of previous IVF treatment cycles
Live birth rates is highest in the first cycle (17.4%) and drop to 14.4% by the fifth cycle (HFEA Report 1999). Although cycles 6-8 appear to give a reasonable chance of success, few patients persevere that long.
| Age group | less than 35 | 35-37 | 38-40 | 41-42 | 43 or over |
| No previous treatments | 33.9% | 27.3% | 18.7% | 11.2% | 3.8% |
| Had previous treatment cycles | 28.5% | 23.7% | 16.1% | 8.7% | 3.7% |
Data adapted from SART report 2002
Previous pregnancy and live birth
Woman, who has been pregnant before or has had a previous IVF birth, has a higher chance of success than woman who has never been pregnant.
The relation between previous pregnancy and live birth and the live birth rate per treatment cycle.
| Previous pregnancy or live birth rate | Live birth rate per embryo transfer cycle |
| Woman has never been pregnant | 12.5% |
| Woman conceived naturally but no live birth | 13.7% |
| Woman conceived naturally and has a live birth | 15.3% |
| Woman conceived by IVF but no live birth | 16.6% |
| Woman conceived by IVF and has a live birth | 23.2% |
Data adapted from HFEA Report 1998.
| Age group | Less than 35 | 35-37 | 38-40 | 41-42 |
| No previous live births | 36.4% | 28.6% | 18.8% | 9.9% |
| One or more live births | 40.3% | 31.4% | 21.6% | 11.9% |
Data adapted from SART report 2005.
The presence of hydrosalpinges
Hydrosalpinges are found between 10 to 30% of couples presenting with infertility due to tubal factor. There is increasing evidence that the presence of hydrosalpinges adversely affects the live birth rates of women undergoing IVF treatment. Live birth rates of infertile women with hydrosalpinges undergoing IVF are reduced by approximately 50% compared to controls. The mechanism for reduced implantation in women with hydrosalpinges is not fully understood but it is possible that the leakage of the fluid from the tube into the womb wash off the embryos, or the fluid itself could have toxic effects on the embryos.
Most specialists offer surgical treatment for hydrosalpinges before IVF treatment. The treatment usually involves removal of the tube (salpingectomy) preferably by laparoscope. An alternative is to occlude the tube at its uterine end again by laparoscopy (clipping the tube) or aspiration of the fluid from the tube. However, These procedars are invasive and carry the risk of injury to bowels, and blood vessels especially in the presence of dense pelvic adhesions (scar tissues). Tubal occlusion from its proximal ends through hysteroscopy using Essure may provide an alternative in these cases.
A recent Cochrane Database Review has demonstrated the efficacy of laparoscopic salpingectomy in improving live birth rates in women with hydrosalpinges due to undergo IVF treatment. NICE Fertility Guidelines in the UK advocates that women with hydrosalpinges should be offered salpingectomy, preferably by laparoscopy, before IVF treatment.
Basal FSH and LH levels (ovarian reserve)
Woman with a base FSH level of 12 or more IU/L or FSH/LH ratio more than 3 or women with an Inhibin level less than 80 pg/ml are unlikely to respond adequately to ovarian stimulation.
Uterine fibroids
Fibroid that compress the cavity of the womb significantly reduce live birth rate (Hart et al 2001 Human Reproduction).
Caffeine consumption
caffeine consumption has adverse effects on the success rates of assisted reproduction procedures, including IVF treatment.
Smoking
Maternal and paternal smoking can adversely affect the success rates of IVF treatment. Smoking reduce implantation and pregnancy rates (Neal et al, 2005,. Human Reproduction). Smoking also adversely affects live birth rates equivalent to increased female age by 10 years (Linsten et al, 2005. Human Reproduction).
Body mass index
Female body mass index should ideally be in the range 19 and 30 before commencing IVF treatment. Female body mass index outside this range is likely to reduce the success of assisted reproduction procedures. Obese women take longer to conceive and are at higher risk of miscarriage than normal weight women.(Linsten et al 2005 Human Reproduction; Fedorcsak et al (2004) Human Reproduction).
Alcohol consumption
consumption of more than 1 unit of alcohol per day reduces the effectiveness of assisted reproduction procedures, including IVF (NICE 2013).
Race
Doctor Luke and colleagues from USA (Journal of Fertility and Sterility,2011) reported lower success rates following infertility treatments in black, Hispanic and Ascian women compared to white women regardless of the weight. Possible causes of this racial difference include fat distribution, also black and Ascian women are more likely to have uterine fibroids.
Previous caesarean section
Women undergoing IVF who have had a previous c-section (CS) have a lower live birth rate than those with a previous vaginal delivery
Emotional distress
Although many infertile couples believe that emotional distress prior to their IVF is a contributing factor to their failure at IVF treatments. Boivin and colleagues reported in the BMJ (2011) that distress is unlikely to affect chances of pregnancy after treatment.