Asherman's syndrome
Asherman's syndrome is the term used to describe the presence of scar tissues (adhesions) between opposing endometrial surfaces inside the womb cavity. The adhesions can be mild or severe, causing significant damage to the womb cavity. Scar tissues inside the womb may interfere with embryo implantation during IVF treatment and ICSI treatment as well as increasing the risk of miscarriage.
Incidence of Asherman's syndrome
The true incidence of Asherman's syndrome is unknown.
Causes
Causes of Asherman's syndrome include:
- Surgical procedures such as myomectomy (removal of fibroids), removal of uterine septum, evacuation of retained products of conception (ERPC), manual removal of placenta (after birth) following childbirth or miscarriage and termination of pregnancy.
- Infection such as tuberculosis or pelvic inflammatory disease (PID).
- Prolonged use of an intrauterine device (IUCD)
Presentation
Women with Asherman's syndrome may have no obvious preblems. The symptoms of Asherman'syndrome depends on the severity of adhesions.
- Diminished menstrual flow or absent periods all together (amenorrhoea)
- Painful periods (dysmenorrhoea)
- Unexplained infertility
- Recurrent miscarriage
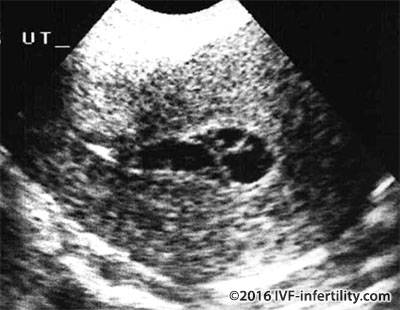
Diagnosis
The diagnosis is primarily made by history (as above). Investigations include saline sonography and HSG. Hysteroscopy, however, is the gold standard of diagnosis and treatment.
Treatment
Surgical removal of scar tissue (Adhesiolysis) is the treatment. The procedure is usually performed with the use of a hysteroscope, which is a safe and effective. The surgeon may place a coil or balloon catheter inside the womb cavity at the end of the procedure to keep the uterine walls apart during the healing process. This will be removed later (4-12 weeks).
Following surgery a 3 month course of hormonal pills (sequential estrogen and progesterone) is usually prescribed to encourage the healing as well as a course of antibiotics to prevent infection. A second-look hysteroscopy may be required to check recurrence.
Outcome of treatment
Hysteroscopic treatment of Asherman's syndrome can dramatically improve both menstrual problem and reproductive outcome. However, pregnancy after treatment remains high risk with complications including spontaneous miscarriage, preterm delivery, intrauterine growth restriction, adherent placenta (accrete) or placenta praevia (low lying placenta), The overall conception rate after hysteroscopic adhesiolysis is about 45% Pregnancy rates appear to depend upon the severity of the adhesions and are higher in mild compared to severe cases. The overall live birth rate is about 30% (Roy et al 2009; Berman 2008). Patients with extensive damage to the endometrium unresponsive to conventional surgical treatment may be offered gestational surrogacy.