What is Polycystic Ovarian Syndrome?
The condition, polycystic ovarian syndrome, known as PCOS, is a common condition and is the commonest cause of ovulation disorders in women of reproductive age and usually present in late teens or early twenties.
Polycystic ovarian syndrome (PCOS), is a primary ovarian condition and is characterized by the presence of many minute cysts in the ovaries, excess production of androgens and menstrual irregularities. Polycystic ovarian syndrome can be found in apparently normal women and the full expression of the disease so-called “Stein-leventhal syndrome” is very uncommon. Polycystic ovarian syndrome is frequently associated with weight gain (only 40-50% of women with PCOS are overweight), excessive hair growth in the face and body, acne (60-70%), irregular and infrequent periods or absent periods, infrequent or absent ovulation, miscarriage and infertility (the risk is higher in women who have few or no periods).
The cause of PCOS is not fully understood. However, PCOS is thought to be a genetic disorder (autosomal dominant) meaning that each child has a 50% chance of inheriting the disorder from a parent who carries the gene. The gene can be inherited from either mother or father. The exact gene causing PCOS has not yet been identified.
There are long-term risks of PCOS including: developing type 2 diabetes, cardiovascular disease and cancer of the womb (three times more likely than women who do not have PCOS). Women diagnosed as having PCOS before pregnancy have an increased risk of miscarriages, developing gestational diabetes, pregnancy induced high blood pressure, pre-eclampsia and pre-term birth. In addition to higher perinatal mortality.
How common is Polycystic Ovarian Syndrome?
The estimated incidence of Polycystic ovarian syndrome (PCOS) varies between 10% to 15% of women of reproductive age, depending on the population studied and the diagnostic criteria applied. PCOS accounts for 90% of women with oligomenorrhoea (infrequent periods) and 30% of women with amenorrhoea (absent of periods) and over 70% of women with anovulation. Rising obesity rates are likely to increase the incidence of PCOS further.
Diagnosis of Polycystic Ovarian Syndrome
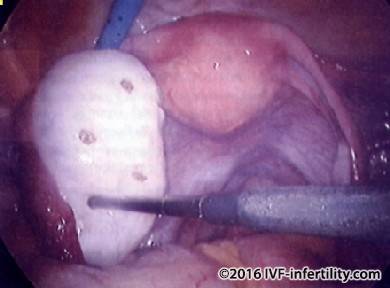
Laparoscopy
Laparoscopy allows direct inspection of the ovaries; the ovaries are enlarged and polycystic. However, polycystic ovaries may appear normal at laparoscopy.
Vaginal ultrasound scan (better than abdominal)
The vaginal ultrasound may show the typical PCOS appearance but reliability varies with expertise.

Blood hormone levels of LH, FSH, androgens and SHBG
Ideally, these tests should be performed during the first four days of the cycle. If the women has no period, then the test can be performed anytime, and repeated if the results do not provide a clear picture.
FSH levels are low or normal, LH levels are often raised (usually slim women). However, a normal level does not exclude diagnosis of polycystic ovarian syndrome (PCOS). Normal or raised estradiol level. The levels of androgens (testosterone, androstendione) may be raised. Raised Anti-Mullerian hormone (AMH). Normal or raised fasting insulin (not routinely measured). Glucose tolerance test (GTT). Prolactin level is usually normal but may be raised in 10% of patients.
The American Society of Reproductive Medicine (ASRM) and the European Society of Human Reproduction and Embryology (ESHRE) joint consensus meeting in November 2003 agreed that the diagnosis of PCOS should be made when two of the following three criteria (Rotterdam Diagnostic Criteria) are met:
- Infrequent or absent ovulation (usually recognised as infrequent or no periods).
- Hyperandrogenism (clinical or biochemical) such as excess hair growth, acne, raised LH, and raised androgen index
- Polycystic ovarian morphology on ultrasound scan (>12 follicles measuring between 2 and 9mm in diameter) and/or ovarian volume >10ml. The distribution of the follicles are not required and with one ovary sufficient for diagnosis.
It is important to exclude other causes of excess androgen before making the diagnosis of PCOS. These include late onset congenital adrenal hyperplasia, ovarian hyperthecosis, Cushings syndrome, and androgen secreting tumours. In general a serum total testosterone level of around 2 to 5 nmol per litre is thought to be consistent with PCOS, while a level higher than 5 nmol per litre should prompt investigation for other causes.
Treating polycystic ovarian syndrome
There is no cure for PCOS so medical management is tailored to the presenting symptoms especially those causing distress to the patients such as acne, hirsutism and infertility in association with lifestyle changes.
Treatment of Polycystic Ovarian Syndrome in women who wish to conceive
Weight loss if she is over weight
This simple measure remains the mainstay treatment for young women with PCOS. It may restore menstruation and ovulation in patients with polycystic ovarian syndrome. Exercise and weight control also reduce the likelihood of developing type 2 diabetes in later life.
Ovulation induction with clomiphene (clomid) tablets
Induction of ovulation with clomiphene tablets is the first choice and is an effective treatment of polycystic ovarian syndrome (PCOS). It results in restoring menstruation and ovulation in about 70% of women and some 30% will conceive within three months of treatment. side effects include mood changes and hot flushes. Clomiphene tablets may be combined with steroid tablets to suppress androgen production. If this fails after a six month trial, then controlled ovarian stimulation with FSH or hMG combined with hCG is used. Because the polycystic ovaries are usually sensitive to stimulation by hormones, it is important to start with a low dose and adjust the dose according to the response. Monitoring of treatment is essential because these patients are susceptible to develop ovarian hyperstimulation syndrome (OHSS) and multiple pregnancy. If the patient failed to respond, one of the following second-line treatments should be considered; depending on clinical circumstances and the patient's preference: laparoscopic ovarian drilling or combined treatment with clomid and metformin if not already offered as first-line treatment or gonadotrophins.
Metformin (Glucophage)
Many women with PCOS have decreased sensitivity to insulin (insulin resistance), and their bodies overcompensate by over-producing insulin. Elevated levels of insulin are common in women with PCOS, whether they are obese or thin compared with weight matched controls. Some experts believe that this excess insulin is the underlying cause of PCOS because insulin stimulates androgen production and effects follicular development. As a consequence, Metformin (oral anti-diabetic drug) combined with Clomid, has been used to treat women with PCOS. Metformin pills is taken daily and usually takes 3 months to start working.
Approximately 15% of women discontinue metformin pills because of unpleasant side effects which are mainly gastrointestinal such as nausea, vomiting, abdominal distension, diarrhoea and unusual tiredness. Long-acting preparations are associated with fewer side effects. Insulin sensitizing drugs have not been licensed in the UK for use in non diabetic patients. Metformin should not be used when kidney function is abnormal.
Initial studies were encouraging; it reported successful restoration of regular menstrual cycles and fertility. More recent large randomised studies have not observed beneficial effects of metformin in the treatment of ovulation problems in women with PCOS although there may be a benefit in specific patients groups such as obese women and women with clomid resistence etc. (Human Reproduction 2008; 23:462-77).
Furthermore, potential benefit from the use of metformin in PCOS women undergoing IVF treatment has been reported.It improves the live birth rates and reduces the incidence of severe ovarian hyperstimulation syndrome (Tange et al, 2006 Human Reproduction).Metformin appears to be safe in pregnancy.
Letrozole
Letrozole is an aromatase inhibitor which acts to prevent oestrogen synthesisis Letrozol can be used as an alternative to clomid. Letrozole is probably associated with higher live birth rates when compared with clomiphene alone and has a better side-effect than clomifene with fewer vasomotor and mood symptoms and may reduce the risk of multiple pregnancy . Letrozole is currently not recommended by NICE as a treatment for infertility in women with PCOS. As for metformin, the use of letrozole for fertility treatment is off-label.
Gonadotrophins
These are powerful and effective drugs and are used to stimulates the ovaries to produce multiple follicles. It is usually offered in selected cases. The use of FSH and hMG should only be performed in clinics that can closely monitor ovarian response; this is because of the increased risk of OHSS and multiple pregnancies. Despite intensive monitoring, multiple pregnancies occur in about 20% of the treatment cycles, of which a third is triplets or more.
Women with PCOS who are being treated with gonadotrophins should not be treatment with gonadotrophin-releasing hormone agonist concomitantly because it does not improve pregnancy rates, and it is associated with an increased risk of ovarian hyperstimulation (NICE 2013).
The Committee on Safety of Medicines in the United Kingdom has advised that no medical products using urine sourced in a country that has reported cases of human variant CJD (the human form of mad cow disease) be used in the UK
Surgery
Surgery is recommended should the medical treatment fail and for women who have experienced OHSS. This may be ovarian drilling or ovarian wedge resection. It is not clear why women with PCOS ovulate after ovarian drilling or wedge resection. After surgery, ovulation occurs spontaneously in 70-90% of women and the probability of pregnancy after one year is in the region of 40-60%. There is no increased risk of multiple pregnancy or OHSS. If ovulatory cycles fail to restore after the surgery, the doctor may restart ovulation induction. A recent study up to 20 years after laparoscopic drilling has shown persistance of ovulation over many years. Compared with medical treatment, it need only be performed once and intensive monitoring is not required. The main problems associated with surgery include adhesion formation, the risk of destruction of the ovaries leading to ovarian failure. In addition, there are risks associated with surgery and anesthesia.
Laparoscopy showing polycystic ovaries

Laparoscopy showing ovarian drilling
Women with polycystic ovary syndrome are at increased risk of pregnancy complications
Women with PCOS are at increased risk of pregnancy complications including pre-eclampsia, giving birth prematurely and developing gestational diabetes while pregnant.Furthermore, Babies born to mothers with polycystic ovarian syndrome were more prone to be large and tended to develop asphyxia during labour (Roos et al, BMJ 2011). Women with polycystic ovary syndrome should be considered "high risk" obstetric patients and should be monitored as such during pregnancy and labour.
Treatment of Polycystic Ovarian Syndrome (PCOS) in women who do not wish to conceive
Menstrual irregularities
Women with irregular and heavy periods are likely to benefit from cyclical hormone treatments. Low-dose combined contraceptive pills(OCP) such as Yasmin and Marvelon are the best option to restore menstrual regularity. It will decrease ovarian hormone production and help reverse the effects of the excessive androgen levels. However, if you smoke and are over 35 years, birth control pills are not recommended. The doctor may prescribe other hormone treatments such as progesterone tablets.cyclic Progestogens such as norethisterone pills to be administered for two weeks every 1-3 months to achieve regular withdrawal bleeds.
Metformin (Glucophage)
Many women with PCOS have decreased sensitivity to insulin, and their bodies overcompensate by over-producing insulin. Elevated levels of insulin are common in women with PCOS, whether they are obese or thin compared with weight matched controls. Some experts believe that this excess insulin is the underlying cause of PCOS because insulin stimulates androgen production and effects follicular development. As a consequence. Metformin pills is taken daily and usually takes 3 months to start working.
Approximately 15% of women discontinue metformin pills because of side effects which are mainly gastrointestinal such as nausea, vomiting and abdominal distension. .
Hirsutism and acne
Hirsutism is best treated with local treatment such as electrolysis, waxing and bleaching. Laser therapy works best for women with dark hair and fair skin, for those with darker skin, it may result in patchy loss of pigmentation at the site of each laser burn.
Vaniqa (EFLORNITHINE) 11.5% cream twice daily application It may be useful in women who wish to avoid hormone treatment. It may also be used in conjunction with hormonal therapy. Improvement may be noticed within 8 weeks. Discontinue if no beneficial improvement within 4 months Side effects include: acne 6%, alopecia 5%, headache, erythema, dry skin etc.
Anti-androgens such as Dianette (ethinyloestradiol and cyproterone acetate). This drug is licensed for moderate to severe hirsutism and severe acne taken for 3 weeks every month. May takes 6-9 months before any improvement is perceived. It may cause liver damage and increase the risk of blood clot. Another anti androgen drug is Spironolactone given in tablet 25-100 mg daily. The drug is advised for women in whom COCP is contradicted.
For acne, some specialists recommend combination of antiandrogen such as Dianette and local cream such as Benzyl peroxide, topical retinoids.