Blastocyst embryo transfer
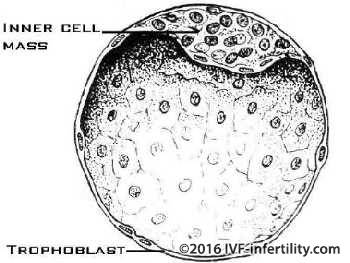
The first IVF human pregnancy was achieved by blastocyst transfer. Blastocyst transfer is claimed to be more physiological than pronucleate or cleaved-embryo transfer is as it mimics nature more closely. As the embryo advances in the development, after 5-6 days it becomes a blastocyst. This has an outer thin layer of cells which will later form the placenta, and an inner cell mass which will develop into the fetus. A blastocyst has about 120 cells.
A blastocyst gives a better idea of the competence of an embryo and has a higher chance of implantation than a cleaved embryo.
In conventional culture medium, about 20% of embryos will develop into blastocysts. Recently, the use of sequential culture medium (the embryos are cultured in different media according to their stage of growth) has enabled a larger number of embryos to develop into blastocysts. However, up to 40% of patients will not grow blastocysts and will not have blastocyst embryo transfer.
The rational behind a blastocyst transfer is that an embryo which has failed to reach the blastocyst stage, would be unlikely to have resulted in a pregnancy. However, if it reaches the blastocyst stage it has about 50% chance of implanting. So the improved implantation rates following blastocyst transfer is due to selection of the best embryos.
Why then do 50% of the blastocysts fail to implant?
A defective blastocyst (e.g. chromosomal abnormalities) is a possible cause; a non-receptive endometrium is another cause.
Blastocyst embryo transfer into the uterine cavity is performed about 5-6 days after egg collection. Transfer of one or two blastocysts is recommended to avoid high-order multiple pregnancies. Supernumery blastocysts can be frozen for future use.
For whom blastocyst transfer is recommended?
-
Patients who had repeatedly failed to achieve a pregnancy following the transfer of good quality cleaved embryos (If the embryo arrest and did not develop to blastocyst, this may indicate a potential egg problem)
-
Patients who wish to achieve a pregnancy without the risk of multiple pregnancy, here the transfer of one blastocyst will be recommended.
- Patient who do not wish to have their spare embryos frozen for whatever reasons may be advised to have blastocyst transfer.
What are the disadvantages of blastocyst trasnsfer?
- About 10% of the embryos that fail to develop to blastocyst in vitro may have done so if replaced inside the womb on day 2 or 3
- Up to 40% of patients will not have blastocyst available for transfer
- Freezing spare blastocyst is not as good as freezing cleaved embryos.
What is the live birth rate following blastocyst embryo transfer?
| Age group | less than 35 | 35-37 | 38-40 | 41-42 | 43 or over |
| Blastocyst transfer | 44.3% | 37.6% | 29.4% | 18% | 7.5% |
| Cleaved embryo transfer | 37.6% | 32.7% | 24.4% | 14.3% | 5.7% |
Live birth rate per treatment cycle using blastocyst transfer. Data adapted from SART report 2000
What is the perinatal outcome of blastocyst transferer?
A sex ratio in favour of males has been associated with blastocyst transfer
There are concerns about the potential deleterious effect of extended embryo culture including imprinting disorders etc. However, after adjusting for co-founding factors, there was increased risk of preterm birth and increased risk of congenital malformations compared with children born after cleaved embryo transfer. Continuing surveillance of children born after blastocyst transfer is therby required.