Management options for tubal damage
There are several possible treatment options available to patients suffering from tubal damage. These may include one of the following techniques: tubal surgery, selective salpingography and IVF.
Tubal surgery
Tubal surgery is performed under a general anesthetic and can be performed by laparoscopy (a keyhole operation) following the surgery. The patient may be able to return home the same day or the following day, returning to full activities in three to seven days. Laparoscopic surgery can be performed using lasers or special instruments. Not all procedures can be performed with this technique. Tubal surgery can be performed by laparotomy, through a cut across the lower abdomen, known as a “bikini incision”. Following laparotomy the patient will usually stay in the hospital for about 3-4 days. When tubal surgery is done by microsurgery (surgery with the aid a special microscope) the results are better.
Your doctor should be able to discuss with you the pros and cons of performing operative laparoscopy versus a laparotomy.The live birth rates after tubal surgery range from 10% for those with severe tubal disease to 70% for those with mild tubal disease.
Some women ask how soon after surgery can they have sex; the answer is as soon as they feel comfortable. Tubal surgery may be appropriate in selected cases where the tubes are not badly damaged. The following are examples of where tubal surgery might be appropriate:
Reversal of sterilization
A small number of women who have been sterilized come forward to request a reversal procedure because of changes in family circumstances. The method used to reverse sterilization will depend on how the operation was initially performed and the extent of damage to the tubes e.g. ligation, clips, rings and diathermy (electrical cautery) etc. The doctor may need to do a laparoscopy and a HSG to assess the status of the tubes before deciding on the operation. Sterilization can sometimes be reversed, however, if the tubes are totally removed or are badly damaged this will not be feasible and your only chance will be IVF. The operation involves the removal of the scarred tissues and rejoining the ends of tubes. The success of such operations is good; but better results are achieved if the operation is performed using microsurgery techniques. The chance that the tubes remain open after surgery is about 80%, and pregnancy rates are about 60%.
Adheisolysis (Salpingolysis)
This involves the division of scar tissues (adhesions) around the tubes. These scars usually glue the tubes to other internal organs causing them to stick together, thus reducing the mobility of the tubes. These adhesions could be due to previous infections or endometriosis. The adhesions are broken down using a special pair of scissors known as microscissors. live birh rates following adhesiolysis is about 50%.
Salpingostomy (neosalpingostomy)
Distal tubal disease account for 85% of the tubal disease. Large hydrosalpinx is treated by removal of the tube (salpingectomy) followed by IVF. Salpingostomy is used to treat a blockage at the fimbrial end (distal end) for mild to moderate hydrosalpinx with normal mucosa of the tube. Any scar tissue that covers the end of the tube is removed; the tube is then opened and turned back on itself so that it will remain open.
The success rate following tubal surgery depends primarily on the extent and site of tubal damage. Other factors that may affect the outcome include: the technique used, women’s age, quality and quantity of male partner sperm and skill of the surgeon. The tube can be opened successfully in 80% of cases, but only about 25% of these women will achieve a pregnancy within a year. This is because when the tube is blocked, much if not all their lining tends to be destroyed, and even if they can be opened by surgery they remain functionless. Furthermore, the scar tissue may return and reblock the tube.
Patients expect tubal surgery to work immediately; this is hardly ever the case. However, if pregnancy has not occurred within 12 months of the surgery, IVF should be considered.
Tubal surgery has the best chance of being successful at the first attempt, repeat tubal surgery is rarely successful and should only be undertaken when other alternatives are not available or unacceptable to the patients. The removal of damaged tubes e.g. Hydrosalpinx prior to IVF treatment has been shown to improve the chance of a live birth.
Salpingectomy (removal of the Fallopian tubes) or tubal occlusion
Women with large hydrosalpinges (Fallopian tube which is blocked at its distal end and distended) should be offered salpingectomy, preferably by laparoscopy, before IVF treatment in order not onlt to improves the chance of a live birth by IVF but also reduce the risk of ectopic pregnancy. If this is not feasible then tubal occlusion is an alternative. There is a risk of reducing ovarian reserve following salpingectomy. The presence of bilateral hydrosalpinx raises ethical dilemma because removing both tubes will render these women entirely dependent on IVF for conception and this does not always succeed. In adddition to the physical, psychological and financial impact of recurrent failed IVF.
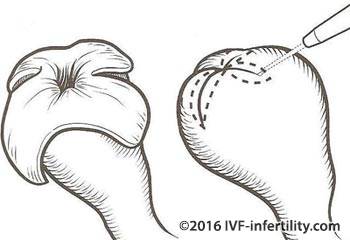
Tubal cannulation
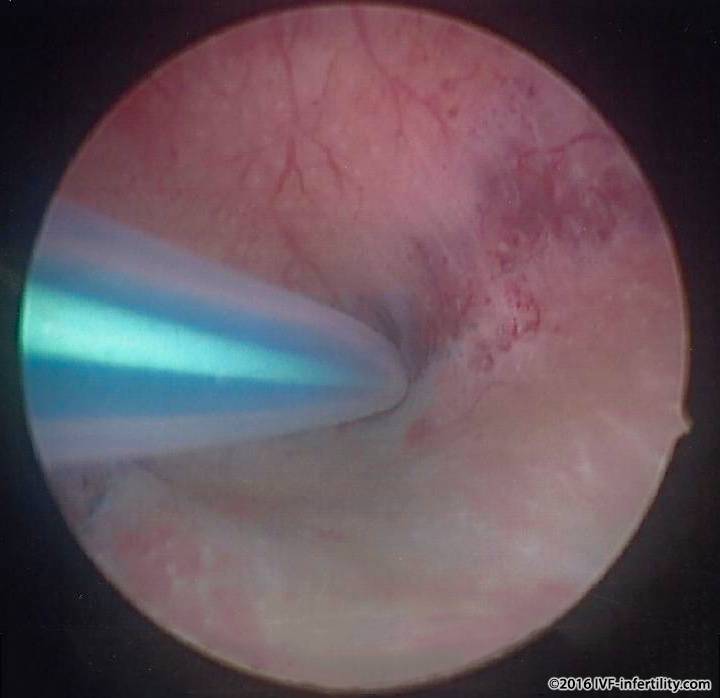
Proximal tubal disease accounts for 15% of tubal factor infertility the occlusions can be mucus or debris which build up over time or scarring from previous infection. The management options include: IVF, and surgery Tubal surgery is performed by either excising the blocked segment of the tube and then re-anastomose the tube to the uterus or cannulaion. Tubal cannulation is simple procedure and is performed through a hysteroscope inserted into the uterine cavity through the cervix (neck of the womb) under a general anaesthestic. It takes between 30-60 minutes. Success rates in opening the tubes is about 80% and the pregnancy rates varies between 30 to 50% the result varies depending on the skill of surgeons with a higher results expected in expert hands. The main complications are perforation of the tube about 1-2% and infection. The patient pay experience pain or discomfort this can be treated with pain killers
Complications of the procedure are minimal and include: perforation of the tube, infection and an increased risk of ectopic pregnancy.and the Fallopian tube may be reblocked
Side effects and complications of tubal surgery
In addition to the general complications associated with any surgery such as: anesthetic complications, infection, bleeding and injury to other organs such as bowels, there are specific complications related to tubal surgery. These include: adhesion formation, reformation of the blockage and ectopic pregnancy. Ectopic pregnancy has been reported to occur in up to 40% of subsequent pregnancies.
Selective salpingography
A procedure used to open the proximal tubal blockage (the end of the tube close to the uterus) when the rest of the Fallopian tube is healthy. Selective salpingography is performed under X-ray control and takes approximately 15-20 minutes. An X-ray dye is injected through the cervix so that the outline of the womb cavity can be seen on the X-ray screen. A special curved catheter is then guided up towards the opening of the tubes and further dye is injected to confirm that the tube is blocked. If the tube is blocked, the dye is injected with a little more pressure in order to remove the obstruction. If this fails, a very fine flexible wire is guided up through the catheter to the opening and gently pushed through. The procedure is not pain free and the patient may feel some discomfort. Selective salpingography has an acceptable success rate. Tubal cannulation is performed through a hysteroscope inserted into the uterine cavity through the cervix (neck of the womb) under a general anaesthestic. It is claimed that the tubes can be opened in up to 90% of cases and up to 50% of women undergoing the procedures are expected to conceive within 12 months. There is a 2% risk of tubal perforation and about 3% risk of ectopic pregnancy. furthermore, the tube may be reblocked.
IVF
The technique IVF is an effective treatment for all forms of ubal damage and pelvic adhesions and should be considered as the first line of treatment for moderate or severe tubal disease. The aim here is to bypass the tubes altogether.
IVF and tubal surgery cost more or less the same and on average result in a similar live birth rates and miscarriage rates. However, ectopic pregnancy is about 10% after tubal surgery compared with 2% after IVF. Multiple pregnancy is about 15-25% after IVF compared with 1% after tubal surgery. Additionally, tubal surgery is associated with a small risk of surgery and anesthesia and Ivf is associated with the small risk of ovarian hyper stimulation syndrome.
Page:1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22